Deep Vein Thrombosis (DVT) Prevention & Treatment: Your Essential Guide
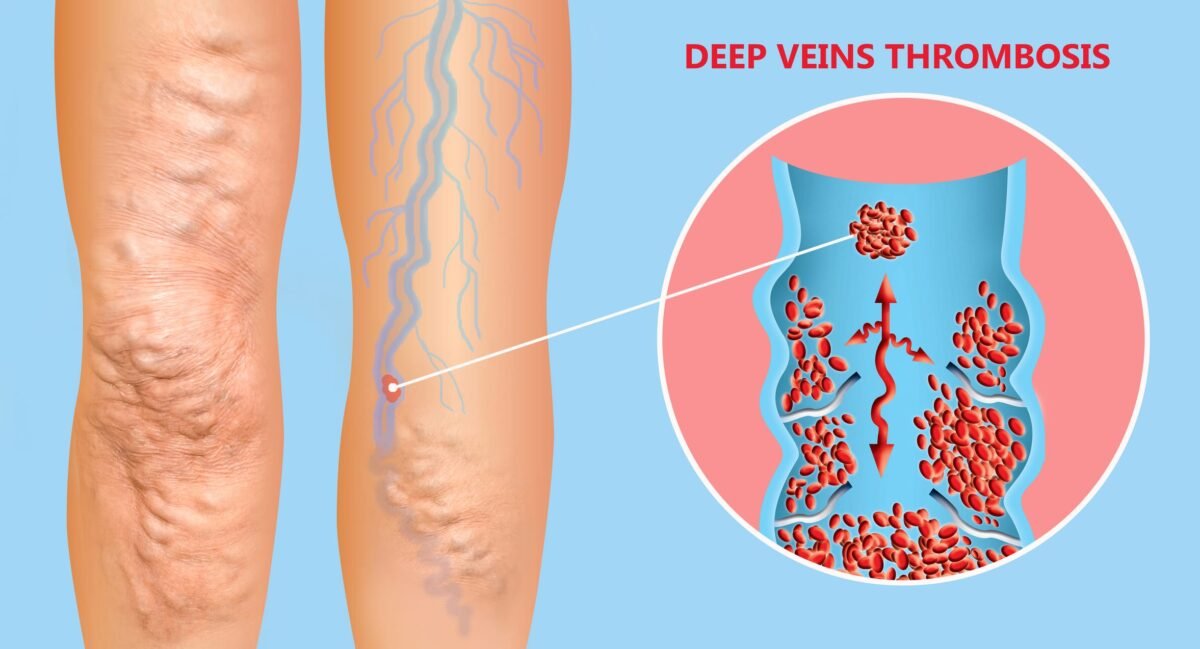
Do you know? Deep Vein Thrombosis (DVT) is a serious condition where blood clots form in deep veins, usually in the legs. If left untreated, these clots can block blood flow and lead to life-threatening complications like a pulmonary embolism (PE). The good news? DVT can often be prevented and managed with the right lifestyle choices and medical care. Understanding the warning signs, risk factors, and treatment options can help you stay safe and maintain healthy circulation.
Delve into the article to know more.
What Is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis (DVT) is a condition where a blood clot forms in one or more deep veins, primarily in the legs. These clots can block blood flow and cause swelling, pain, and complications like pulmonary embolism if they travel to the lungs.
Understanding the Roots: What Causes Deep Vein Thrombosis?
DVT doesn’t just happen randomly. It typically results from factors that slow blood flow, damage a vein wall, or make the blood more likely to clot. Medical professionals often refer to Virchow’s Triad to explain these contributing factors:
- Stasis (Slow Blood Flow): When blood flow in the veins slows down or stagnates, clots are more likely to form. This is common during periods of prolonged immobility, such as:
- Long journeys (flights, car rides, train travel) where you sit for extended periods
- Bed rest due to illness, surgery, or injury
- Paralysis or limited mobility
- Hypercoagulability (Increased Clotting Tendency): Certain conditions or factors can make your blood thicker or more prone to clotting:
- Inherited blood clotting disorders (e.g., Factor V Leiden)
- Hormone therapy or birth control pills containing estrogen
- Pregnancy and the postpartum period (up to six weeks after birth)
- Certain cancers and their treatments (chemotherapy)
- Dehydration
- Inflammatory diseases like Crohn’s disease or rheumatoid arthritis
- Smoking
- Endothelial Damage (Vein Injury): Damage to the inner lining of a blood vessel can trigger clot formation. This can occur due to:
- Surgery, particularly major operations involving the hips, knees, or abdomen/pelvis
- Significant trauma or injury, like fractures
- Catheter placement or other invasive vascular procedures
- Chronic inflammation or infection near a vein
Other Risk Factors:
- Age: The Risk increases significantly after age 50, though DVT can occur at any age.
- Obesity: Being overweight or obese puts extra pressure on the veins in your legs and pelvis.
- Personal or Family History: Having had a DVT or PE before, or having close family members who have, increases your risk.
- Varicose Veins: While typically superficial, severely twisted and enlarged veins can sometimes be associated with a slightly increased risk of DVT.
Recognising the Danger: What are the First Warning Signs of DVT?
It’s crucial to know the symptoms, as early detection significantly improves outcomes. DVT symptoms and treatment are closely linked – recognising symptoms prompts seeking treatment. About half of people with DVT have no noticeable symptoms. However, when symptoms do occur, they usually affect one leg (or arm, though less common) and can include:
- Swelling: This is often the most common sign, occurring in the affected leg, ankle, or foot.
- Pain or Tenderness: Often described as a cramping or soreness, similar to a pulled muscle. The pain might only be felt when standing or walking.
- Warmth: The skin over the affected area may feel warmer than the surrounding skin.
- Redness or Discoloration: The skin might appear reddish or bluish.
- Visible Veins: Surface veins may become more prominent or swollen.
One patient shared, “After a long flight, I thought I had just pulled a muscle in my calf. It was sore and a bit swollen, so I didn’t see a doctor right away. But when it turned warm and red, I remembered it could be a sign of DVT. I went to Dr. Mittal, and he confirmed it. We started treatment immediately. If I had waited longer, it could have been dangerous.”
Warning Signs of Pulmonary Embolism (PE) – Seek Immediate Emergency Care
If a clot travels to the lungs, it can cause:
- Sudden shortness of breath
- Sharp chest pain, often worse with deep breaths or coughing
- Rapid heart rate
- Coughing, potentially with bloody sputum
- Lightheadedness, dizziness, or fainting
- Unexplained anxiety
As Dr. Dinesh Mittal highlights, “Recognising the first warning signs of DVT and seeking immediate medical evaluation is not just advisable, it’s potentially life-saving. Timely treatment for deep vein thrombosis drastically reduces the risk of dangerous complications like pulmonary embolism.” If you suspect DVT or experience PE symptoms, seek medical attention without delay.
Proactive Measures: Essential Steps for Deep Vein Thrombosis Prevention
While you can’t eliminate all risks, you can take significant steps to lower your chances of developing DVT, especially if you have known risk factors or are facing a period of immobility. Effective deep vein thrombosis prevention includes:
- Stay Active & Move Regularly:
- Avoid Prolonged Sitting/Standing: Get up and walk around every 1-2 hours. If you’re stuck sitting (like at a desk or on a plane), do leg exercises.
- In-Seat Exercises: During long periods of sitting, perform calf raises (point toes up, then down), ankle circles, and foot pumps regularly.
- Post-Surgery Mobilization: Follow your doctor’s advice about getting up and moving as soon as possible after surgery or illness.
- Regular Exercise: Maintain a healthy lifestyle with regular physical activity appropriate for your fitness level.
- Travel Smart:
- On long journeys (over 4 hours), get up to walk the aisle or stop the car frequently to stretch your legs.
- Perform the in-seat leg exercises mentioned above at least every hour.
- Wear loose-fitting clothing.
- Stay well-hydrated.
- Consider wearing graduated compression stockings, especially if you have risk factors.
- Stay Hydrated: Drinking plenty of water helps keep blood thinner and flowing smoothly. Avoid excessive alcohol or caffeine, which can contribute to dehydration.
- Maintain a Healthy Weight: Losing excess weight reduces pressure on your veins.
- Quit Smoking: Smoking damages blood vessel linings and increases clotting risk.
- Compression Stockings: These specially fitted stockings are tightest at the ankle and gradually decrease in pressure up the leg, helping to improve blood flow. They are often recommended during long travel, pregnancy, after surgery, or for individuals with a history of DVT. Consult your doctor about the right type and pressure level.
- Medication (Anticoagulants): For individuals at high risk (e.g., after major surgery, with a history of clots, or during cancer treatment), doctors may prescribe blood-thinning medications as a preventive measure. Always take these exactly as prescribed.
Dr. Dinesh Mittal further advises, “Consistent preventive measures are key, especially for those with known risk factors. Even simple actions like regular movement during travel or post-surgery can significantly lower the chance of developing a clot. It’s about being proactive about your vascular health and discussing your risks with your doctor.”
Medical Approaches: How to Treat Deep Vein Thrombosis
If you are diagnosed with DVT, prompt treatment is essential to prevent the clot from getting larger, breaking loose (causing a PE), and reducing the risk of long-term complications. How to treat deep vein thrombosis primarily involves:
- Anticoagulants (Blood Thinners):
- Role: These are the cornerstone of DVT treatment. They don’t actually dissolve existing clots but work by preventing new clots from forming and stopping the current clot from growing larger. This gives the body time to break down the clot gradually.
- Types: Common anticoagulants include injectable heparin (often used initially in hospitals), low-molecular-weight heparin (LMWH, injections you might give yourself at home), warfarin (an older oral medication requiring regular blood monitoring), and newer direct oral anticoagulants (DOACs like apixaban, rivaroxaban, dabigatran, edoxaban) which often don’t need frequent monitoring.
- Duration: Treatment typically lasts for at least 3 to 6 months, but depending on their risk factors and history, some people may need lifelong anticoagulation.
- Thrombolytics (Clot Busters):
- Role: These powerful drugs actively dissolve blood clots.
- Usage: They are reserved for very severe cases of DVT (e.g., massive clots causing significant limb threat) or for treating life-threatening PE due to a higher risk of severe bleeding. They are usually administered in a hospital setting.
- Inferior Vena Cava (IVC) Filters:
- Role: In specific situations where anticoagulants cannot be used (e.g., active major bleeding) or are ineffective, a small filter may be surgically placed in the large vein (vena cava) in the abdomen.
- Function: This filter catches blood clots traveling from the legs, preventing them from reaching the lungs and causing a PE. It doesn’t treat the DVT itself, and these filters are often intended to be temporary.
- Graduated Compression Stockings: Often recommended during and after DVT treatment to improve blood flow, reduce swelling and pain, and potentially lower the risk of long-term complications like post-thrombotic syndrome (PTS).
Another individual successfully treated by Dr. Dinesh Mittal recalls, “Being diagnosed with DVT was frightening, but Dr. Mittal and his team explained the treatment plan clearly. Taking the blood thinners became routine, and wearing the compression stockings really helped with the swelling. Seeing the clot resolve on follow-up scans was a huge relief. I’m much more aware now and follow all the prevention advice diligently.”
What Is The Cost Of Deep Vein Thrombosis Treatment In India?
The cost of treating Deep Vein Thrombosis (DVT) in India can vary significantly based on several factors: the city and hospital chosen, the severity of the DVT, the specific treatments required (e.g., type and duration of anticoagulants, need for hospitalisation, potential procedures like thrombolysis or filter placement), diagnostic tests, and the duration of follow-up care. Generally, costs range from approximately INR 30,000 to INR 2,50,000 (around 360 to 3,000 USD) or potentially higher for complex cases requiring interventions or extended hospitalisation. This range covers initial diagnosis, medications, and standard follow-up. Procedures like thrombolysis or IVC filter placement would add substantially to the cost. It’s best to get a detailed estimate from the chosen healthcare provider.
Conclusion
Deep Vein Thrombosis is a serious condition, but awareness and proactive steps can make a significant difference. Understanding what causes deep vein thrombosis, recognising the first warning signs of DVT, and adopting effective deep vein thrombosis prevention strategies are crucial. If DVT does occur, knowing how to treat deep vein thrombosis promptly and effectively with medical guidance is essential to prevent life-threatening complications like pulmonary embolism and long-term issues like post-thrombotic syndrome. Maintain an active lifestyle, be vigilant about symptoms, especially during high-risk periods, and never hesitate to consult a specialist if you have concerns.
FAQs
1. How Long Does It Take For A DVT Clot To Dissolve?
It depends on the severity and treatment plan, but with proper care, clots typically dissolve within a few weeks.
2. Is DVT Only A Concern For Older adults?
No, DVT can affect people of all ages, especially those with risk factors like obesity, pregnancy, or prolonged immobility.
3. Can DVT Go Away On Its Own?
DVT rarely resolves without treatment and can lead to complications if ignored. Medical intervention is essential.
4. What Foods Should I Avoid If I Have DVT?
Limit processed foods, excessive salt, and unhealthy fats. Stick to a balanced diet rich in fiber, omega-3s, and antioxidants.
5. When Should I See A Doctor for a Possible DVT?
If you notice swelling, pain, redness, or warmth in one leg or experience shortness of breath, seek medical attention immediately.
Explore more blogs: Heart Bypass Surgery (CABG): Procedure and Recovery Time