What is a Blalock shunt procedure?
Pediatric cardiac interventions encompass a range of procedures aimed at diagnosing and treating heart conditions in children. The complex nature of congenital heart defects presents significant challenges, affecting growth and development. The BT Shunt procedure, introduced by Dr. Alfred Blalock in the 1940s, marked a pivotal advancement. It provided a lifeline for infants with severe heart defects, creating a temporary connection between arteries and allowing vital oxygenation.This procedure revolutionized pediatric cardiac care, offering a bridge to life-saving surgeries for these vulnerable infants, ultimately shaping the field and setting the stage for further advancements in the treatment of congenital heart conditions.
The BT shunt stands for the Blalock-Thomas-Taussig shunt, often referred to solely as the Blalock-Taussig shunt. It is named after those who helped create it — Alfred Blalock (surgeon), Helen B. Taussig (cardiologist), and Vivien Thomas (lab technician).
It is a lifesaving procedure in the world of pediatric cardiac interventions. Picture this: it’s like nature’s emergency bridge for newborn hearts. When the vital “ductus arteriosus” decides to close shop too early, leaving tiny hearts gasping for oxygen, the BT Shunt steps in as the ultimate savior.
These shunts aren’t lifelong friends but more like loyal sidekicks on a rescue operation. And the best part: With a success record of 82.0%, it is a light of hope for apprehensive parents.
What is Blalock- Taussig Shunt?
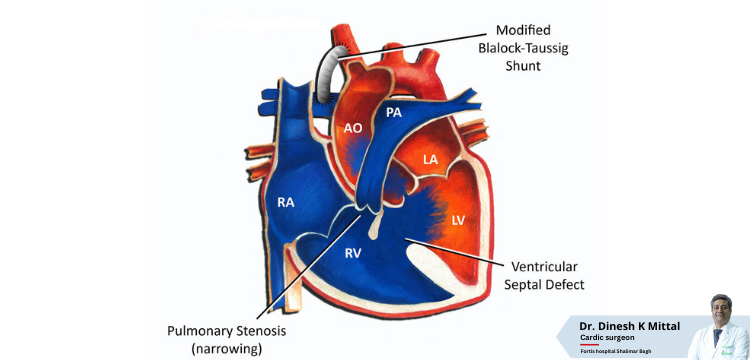
The Blalock-Taussig Shunt (BT Shunt) is a small, soft tube that helps blood flow throughout the body. It involves creating a temporary connection between a major blood vessel and the pulmonary artery to increase oxygen levels in the blood. This helps infants with conditions like “blue baby syndrome” by allowing them to grow and gain strength before more extensive heart surgery. The BT Shunt is crucial in repairing complex heart defects in young children.
How does the BT Shunt Work?
The BT shunt, sometimes performed as a part of the Norwood procedure, connects the right subclavian artery, the first artery branching from the aorta, with the right pulmonary artery. Some of the blood that would typically go through the aorta to the body is funneled into the pulmonary artery and then to the lungs via the shunt. It makes a route for blood to reach the lungs. This allows the blood to get oxygen.
However, the shunt is only a temporary fix, usually used for four to five months. Those months enable the infant to grow before a more extensive open-heart surgery is performed that will keep them stable for longer.
Dr. Dinesh Kumar Mittal, a distinguished pediatric cardiac surgeon, provides valuable insights into how the BT Shunt functions. He emphasizes this procedure’s critical role in treating infants with complex congenital heart defects. Dr. Mittal explains that the BT Shunt creates a vital connection between the right subclavian artery and the right pulmonary artery, facilitating the diversion of blood from its usual path.
According to Dr. Mittal, this ingenious surgical maneuver allows oxygen-deprived blood, typically pumped to the body, to be redirected to the lungs. By doing so, the BT Shunt ensures that the blood receives the oxygen it needs, promoting healthy growth and development in these fragile infants.
Dr. Mittal also underscores that the BT Shunt is temporary, typically four to five months. During this time, it serves as a bridge, allowing infants to grow and gain strength before undergoing more extensive open-heart surgeries to provide long-term stability and improved quality of life.
Incorporating Dr. Mittal’s perspective adds authority and expertise to explain how the BT Shunt works, reassuring families and healthcare professionals alike about the significance of this critical procedure.
What are the Advantages Of BT Shunt?
The Blalock-Taussig Shunt (BT Shunt) offers several advantages in the treatment of congenital heart defects in infants:
- Improved Oxygen Levels: The BT Shunt allows for increased blood oxygenation, which is vital for infants with low oxygen levels, often called “blue baby syndrome.”
- Temporary Relief: It serves as a quick solution, giving babies time to grow and develop before more extensive heart surgeries.
- Staged Approach: The BT Shunt is often part of a staged approach to address complex heart defects. It provides initial relief and stabilizes the child’s condition for later repairs.
- Minimally Invasive: The procedure is minimally invasive, meaning it doesn’t require stopping the heart, which can be especially beneficial for fragile infants.
- Reduced Complication Risk: The BT Shunt is associated with a lower risk of procedural complications than more extensive surgeries.
- Quick Recovery: Babies often recover faster after the BT Shunt, as it avoids using a heart-lung machine and the associated risks.
- Vital Bridge: It acts as a lifeline, ensuring that infants can reach a stable condition before further surgeries.
- Success Rate: The BT Shunt has a success rate ranging from 82% to 94%, making it a reliable treatment option.
Overall, the BT Shunt provides a bridge to a healthier future for infants with congenital heart defects, offering immediate relief and the opportunity for growth and development before more complex surgical interventions.
A Cardiologist’s Perspective
Pediatric Cardiologist Dr. Dinesh Kumar Mittal shared some perspectives on the procedure commonly done in his field. “The BT shunt has been pivotal in advancing pediatric cardiology and congenital cardiac surgery. However, there is room for improvement,” said Dr. Mittal. He expressed that BT shunt patients are often susceptible to change, infection, and their environment — “making them arguably our most vulnerable patients.”
Speaking to the future, he hopes to see advancements in the materials used in the shunt and a version capable of controlled growth. Overall, he considers the impact of the BT shunt and the improvements that have come over the years but sees opportunities for a better procedure.
“There is a growing experience with [PDA] stent placement in place of BT shunt placement in certain infants. PDA stent patients encounter a lower risk of procedural complications and shorter intensive care unit length of stay.” The PDA stent has the same survival rates as the BT shunt but with fewer complications.
BT Shunt After Care
Blalock-Taussig (BT) shunt care after surgery will include:
- Mechanical ventilation — a breathing machine — immediately following the operation
- Chest tubes to collect fluid that can accumulate in the chest
- Foley catheter to collect urine and accurately keep track of urine output
Many children with a BT shunt must be closely monitored at home. The healthcare team provides the monitoring equipment, trains you to use it, and continually checks in on your child until they are ready for the next operation.
Thus, the Blalock-Taussig Shunt has become a remarkable procedure for infants with heart defects. It’s like a bridge to a healthier life. This minimally invasive surgery improves oxygen levels, providing temporary relief and reducing complications. While it’s been a lifesaver, there’s always room for improvement.
Read Also : VSD Closure Treatment and Cost in Delhi NCR | Dr. Dinesh Kumar Mittal